Exclusive : Administrative Failure, Not Just Oxygen Cut, Caused Gorakhpur Hospital Tragedy, Says Govt Panel
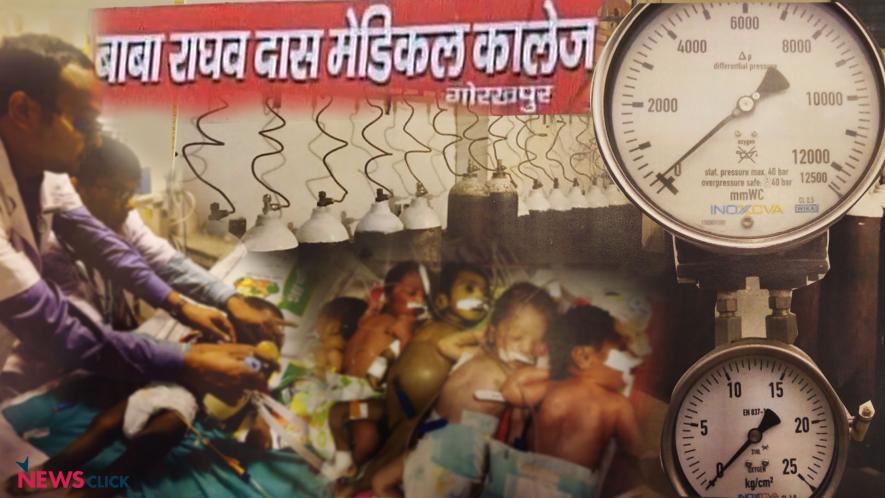
Systematic administrative failure, not just disruption of oxygen supply, caused the deaths of over 30 children at Baba Raghav Das (BRD) Medical College of Gorakhpur in Uttar Pradesh on the intervening night of August 10-11, 2017, revealed a high-level probing team of doctors constituted by JP Nadda, Union Minister of Health and Family Welfare.
Inadequate number of doctors, inadequately trained nurses, overcrowding of infant beds with 4-5 newborns on each, disregard of asepsis principles and too much pressure on facilities were listed with photographic evidence in the chilling report, which has not been publicly released, but was accessed and reviewed by Newsclick exclusively.
The report puts paid to the oxygen supply cut reason popularized by the state govt. and the media, and thus exposes the error of blaming doctors for not arranging oxygen. The picture that emerges is of systemic negligence of the hospital for which the state govt.’s health department and policy makers appear to be solely responsible.
The team consisting of Dr MK Aggarwal, Deputy Commissioner (Immunisation) at Ministry of Health and family Welfare; Dr Harish Chellani, professor and head of pediatrics at VMMC and Safdarjung Hospital, New Delhi; and Dr Sushma Nangia, director, professor and head of neonatology at Lady Hardinge Medical College and Associated Hospitals, New Delhi visited BRD College on August 13, 2017 – two days after the incident. Based on records review, interaction with healthcare providers and onsite evaluation of the infrastructure, equipment, human resource and hospitalised children it carried out a comprehensive day-long evaluation and submitted its report to the ministry on August 15 last year.
The high-level inquiry panel found that the admissions and deaths between August 1 to August 6, 2017 and that between August 7 and August 12, 2017 were “not different”.
“As per the data made available by the state, it was observed that there was no increase in number of deaths in the period 24 hours before (18) and 24 hours after (11), so also the number of deaths in the period 48 hours before (36) and 48 hours after (35), the alleged period of interrupted oxygen supply (from the evening of August 10 to morning of August 11, last year),” said the report.
There was no increase in deaths in July 2017 when compared to July 2016. In fact, the numbers were lower – 292 vis-a-vis 200, said the report.
The report made a chilling revelation that “there was gross overcrowding in the Neonatal unit, both in the extramural and the intramural sides, with each bassinet housing 4-5 neonates instead of one”.

“Extramural admissions were more than intramural and deaths were higher in extramural babies as against intramural ones,” it said adding that “during the first half of this year (January-June 2017), there were 1,548 outborn as against 521 inborn admissions in the neonatal unit with 42% and 33% deaths respectively”.
The report also talked about gross administrative failures that may have contributed to the emergency situation on the fateful night and doctors allegedly being made scapegoats to cover the lapses.
The report says, “The overall strength of faculty and junior residents (pursuing MD), including non-academic JR (junior residents) seems reasonable; however, the number of senior residents (post MD residents) is grossly inadequate being 4 against 12 vacancies and they need to be on the floor to provide 24X7 cover and not just during routine hours,” it said.
It is these post MD senior residents who take decisive actions as regards patient care and make a significant difference in the quality of care provided to the patients. “Currently, the patients are managed beyond the routine hours by junior residents who are themselves still students and learning to manage sick patients,” the team found.
Though nursing personnel are adequate in number, yet they are not trained to care newborn, the report said. “Nursing personnel are adequate in number but they need to be rationally deployed round the clock to provide optimum care. In addition, nurses trained in care of newborn are negligible. Out of 31 nurses working in neonatal area, only 3 are FBNC (facility based newborn care) trained,” said the doctors’ panel.
Adding that clinical management protocols of neonatal patients need to be strengthened and augmented, the doctors’ team found that “there is suboptimal care with regard to asepsis (the absence of bacteria, viruses and other microorganism) routines such as hand-washing, use of disinfectants, cleaning of bassinets after discharge or death of neonate”.
The doctors found that there was “gross overuse of antibiotics and intravenous fluid therapy as well as poor nutritional support in form of enteral feeding”.
This is further substantiated by the fact that during this period (1-12 August, 2017), 30% neonates and 13% paediatric case died. Deaths early after admission (within 12 hours) were just 11%, with 25% within 24 hours of admission and another 25-35% deaths thereafter, in the next 24 hours. This indicates that nearly 50% deaths occurred within 48 hours of admission “implying both suboptimal stabilisation at peripheral units and poor care after admission in the BRD Medical College”.
The experts also found that the parents of the neonates have to buy consumables and a number of disposables, which is the responsibility of the hospital. “There is out of pocket expenditure as parents of neonates have to buy many disposables and consumables for neonatal patients although the same for acute encephalitis syndrome (AES) patients is taken care by the hospital supply,” the experts said in their report.
The pressure on doctors in understaffed BRD Medical College can be gauged by the fact that number of referrals to the hospital – both for pediatrics and neonatal cases – is high, possibly because this is the only tertiary facility available in the region. There were 175 pediatric and 70 neonatal admissions with 16% pediatric deaths and 49% neonatal deaths during August 1-6, 2017.
Similarly, during August 7-12, in the last year, there were 188 pediatric and 99 neonatal admissions with 16% pediatric and 42% neonatal deaths. Most neonatal deaths were due to ‘asphyxia’ (lack of oxygen to the brain), prematurity and sepsis; whereas, most pediatric deaths were as a consequence of ‘acute encephalitis syndrome’.
These findings lend credence to the allegations that the doctors are being made scapegoats for the failures of govt. negligence.
Get the latest reports & analysis with people's perspective on Protests, movements & deep analytical videos, discussions of the current affairs in your Telegram app. Subscribe to NewsClick's Telegram channel & get Real-Time updates on stories, as they get published on our website.