'Oxygen Surveillance': Rethinking A Welfare State

Representational Image. Image Courtesy: AFP
A lack of anticipation by the Central Government has accentuated a deadly second wave of COVID-19 resulting in a death toll which can only be estimated at the moment. The Centre's misplaced priorities hurled the nation into an abyss with a severe Oxygen crisis where hapless Indians cried out for Oxygen and stormed social media with the hashtag #IndiaCantBreathe.
But Kerala's trajectory stands out in the rest of the country at this time. Even though there has been a huge spike in cases, the state had an “oxygen surplus” and low death rates. This necessitates the economist Kenneth Arrow’s thesis 'Uncertainty and the Welfare Economics of Medical care'. Written in 1963, it emphasised on rethinking the contours of a welfare state.
1,500 Oxygen Beds: A Milestone Step
In this unprecedented situation, the public health system is faced with uncertainty and asymmetric information. The government of Kerala’s foresight helped it to stabilise the surge in COVID-19 cases. In 2019, Kerala depended mainly on neighboring states for liquid oxygen. But lessons were learned from the first wave and its daily oxygen stock has risen from 99.3 metric tonnes in April 2020 to more than 219 metric tonnes at the time of writing.
Within a year, the government augmented oxygen capacity by around 60%. This stock of oxygen is effective in catering to the demands of the health sector. With the alarming situation given the rise in cases, the government recently started Oxygen war rooms in all districts. India’s biggest Oxygen bed facility was also started at Amabalamugal, Ernakulam, which has a capacity of 1500 beds
Chart: Date-Wise Reporting of COVID-19 Cases over 30 Days
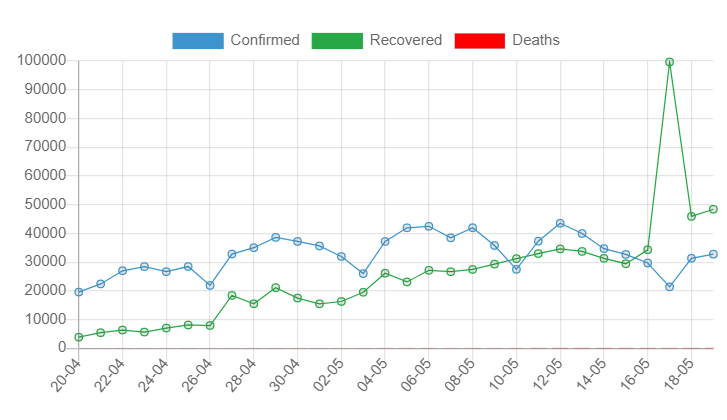
Source: dashboard.kerala.gov.in
Unlike other states, Kerala's Test Positivity Rate (TPR) was around 23.3%, which is quite high a number. The demographic vulnerability of its dense population has always posed a challenge to the state. Despite a huge spike in COVID-19 cases a high recovery rate of 87.22% and an abysmally low death rate of 0.3 per cent shows the efficiency of Kerala's public health system. Among districts, Ernakulam has emerged as an epicentre of cases. Due to the population concern, the state government has set up a temporary COVID hospital with 1,500 beds in association with local self-government and BPCL (Bharat Petroleum Corporation Ltd). Being India’s biggest Oxygen bed facility, it has a direct and uninterrupted supply of oxygen.
“BPCL is providing oxygen and utilities free of cost and has a maximum production capacity of 24 tonnes per day. Thus, around 90% of patients can recover with the help of this support under the supervision of a large number of doctors and nurses,” said Prince George, Deputy Manager, BPCL.
The Out Of Pocket Expenditure (OOPE) in the health care system remains high for a lot of socio-economic groups. It is disheartening to see, that in many states, private agencies are selling Oxygen cylinders at an exorbitant price. This not only marks a high OOPE but also reduces the common person's means of subsistence. Undoubtedly, an increase in the government’s public health expenditure on social welfare measures helped to regulate social harmony in a society divided on class lines.
Kerala Arogya Suraksha Padhathi's (KASP) – a health care scheme which provides Rs five lakh insurance cover per family each year – beneficiaries and government referred patients can avail free treatment from private hospitals. This helped to maintain and to keep a check on OOPE even in times of crisis. Grassroots-level democracy and behavioural responses of people in times of a crisis play a vital force in any new initiatives by the government.
Decentralized Planning and Digital Oxygen War Room
Delivery of oxygen alone doesn’t serve the entire needs of a state. To monitor demand and distribution of the supply, “Oxygen war rooms” have been set up across all districts to manage the total inflow of patients. The war room operates round-the-clock and is monitored by district collectors. A task force comprising various public health experts, civil servants, epidemiologists from Harvard T.H. Chan School of Public Health, and data analysts are in charge of coordinating these activities. The data is compiled by a special software called 'CoronaSafe Network' to ensure efficiency and equity in the health sector. Decentralised patient management helps in achieving care and attention at the ward level which retains public confidence.
“The well-integrated system helps in real-time oxygen monitoring, project burn rate, and time to empty liquid oxygen. Integrated telemedicine, triage and ambulance shifting helps to avoid the informational inequality that people face in a typical health market,’’ said Aparna Sathyanathan, Head of Emergency Network Operations.
National Apathy and Lessons
The political incompetence of the incumbent regime turned this pandemic's second wave into a man-made catastrophe. The laxity of the Centre towards public health care is reflected in the Union Budget which allocated considerably lesser than what was envisaged by the National Health Mission. In a country where a large section of lower-income households gasp for Oxygen, the Centre must actively intervene rather than behaving like a student who wakes up late for an examination. In India, social distancing and handwashing are privileges that are not affordable for the lower middle class and beyond. A vast majority of communities are deprived and excluded from basic healthcare.
A comparison between the Central Government’s policies and those by Kerala resembles a divergent road. In Kerala, medical items which are necessary for COVID-19 treatment were made essential articles under the Kerala Essential Articles Control Act, 1986, and a maximum retail price was fixed. The bare minimum that a government can do is to ensure zero-rated GST on medical items, especially on Oxygen. Sadly, the Centre’s regressive taxation policies further deepen the inequality and left the poor to bear the brunt of an economic fallout. Rather than increasing public expenditure, the government is providing a friendly atmosphere for private capital accumulation in the health sector. Prima facie, ensuring mass vaccination is the only solution, but hardly three per cent of the total population has been fully vaccinated so far. Not an 'Act of God', only stringent measures can break the vicious cycle of a deadly pandemic.
The writer is a student of Economics at Jawaharlal Nehru University, New Delhi. The views are personal.
Get the latest reports & analysis with people's perspective on Protests, movements & deep analytical videos, discussions of the current affairs in your Telegram app. Subscribe to NewsClick's Telegram channel & get Real-Time updates on stories, as they get published on our website.